Help us protect the commons. Make a tax deductible gift to fund our work. Donate today!
You’ve heard the stories: engineers 3D printing face shields in their basements; do-it-yourself hobbyists sewing face masks; and fashion designers crafting personal protection gowns.
Globally, people are trying to help fill the medical supply gap caused by the COVID-19 pandemic through open-source medical hardware. It’s a heartwarming display of global ingenuity, innovation, and collaboration. In this post, we answer your questions about open-source medical hardware and provide some insight into what you can do to help.
Open-source hardware: the designs of physical objects that are openly licensed so they can be modified, created, and distributed without restrictions.
Why is open-source medical hardware important?
It’s easy to forget, with such a flurry of increased activity, that open-source medical hardware is not new. In fact, it has been instrumental in providing medical devices and equipment to under-resourced healthcare workers and facilities for years—a need that predates the COVID-19 pandemic. For example, following the H1N1 pandemic, medical professors at Swansea University published open-source instructions for a low-cost emergency ventilator.
In a 2010 report titled, “Managing the Mismatch,” the World Health Organization (WHO) stated, “Research is making rapid progress within the development of sophisticated medical technologies…Yet despite this progress, the majority of the world’s population has little or no access to many of these innovations.” In particular, the WHO detailed a significant “mismatch” in the availability of relevant, effective medical devices for localized public health needs, highlighting that “70–90% of all medical devices donated to the developing world never function as intended.” Four important components of correcting this “mismatch” are availability, accessibility, appropriate(ness), and affordability—this is where open-source medical hardware comes in, as Dr. Gerrit Niezen et. al. explained in a 2016 research article:
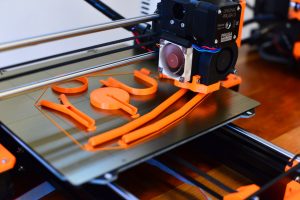
A 3D printer builds a stethoscope using The Glia Project’s open-source design. Source: The Glia Project (CC BY-SA)
“Making the hardware design available under an open source license allows anyone to improve and contribute to the device design, leading to very rapid innovation compared to traditional methods. It also enables the design to be modified for very specific uses, and makes the devices easy to repair…This has great potential for making medical devices more accessible in the developing world, where devices can also be designed as open-source and built for specific use cases, instead of having to depend on donated equipment.”
A clear example of a medical device “mismatch” is the cost of a stethoscope compared to its necessity. Although stethoscopes are one of the most important tools for healthcare workers, on the market, a reliable stethoscope costs between $90.00 – $200.00 USD and is almost impossible to come by in low-resource settings. After noticing this issue while working in Gaza, Dr. Tarek Loubani, an emergency room physician in Canada and recipient of the 2020 Bassel Khartabil Fellowship, created an open-source design for stethoscopes in 2018 that can be 3D printed for around $3.00 USD. Through his charity, The Glia Project, Dr. Loubani now creates and releases open-source designs for stethoscopes, tourniquets, and otoscopes so that they can be produced cheaply by anyone with a 3D printer. The charity not only creates these designs, they also train people in under-resourced and conflict-ridden areas to use 3D printers and deploy these medical devices in the field. “The Glia Project is first and foremost a project about independence,” explained Dr. Loubani in a 2019 interview.
Just recently, in response to the pandemic, the organization turned to creating face masks for Canadian health workers. “That’s been my promise to my colleagues,” Dr. Loubani recently told the CBC, “And soon that will be my promise to all health-care workers in Canada.”

Creating open-source medical hardware during the COVID-19 pandemic
Dr. Loubani is not alone in using open-source hardware to mitigate the medical supply and equipment shortage due to COVID-19. The Helpful Engineering Group on Slack is filled with thousands of engineers crowdsourcing ideas for medical devices and tools, and the Open Source COVID-19 Medical Supplies (OSCMS) group on Facebook has over 50,000 members doing the same. Alongside these somewhat ad hoc and loosely organized efforts are initiatives by research institutions and labs, such as the MIT Emergency Ventilator (E-Vent) project and the Just One Giant Lab OpenCovid19 Initiative.
What’s the manufacturing process?
The process of identifying an open-source hardware design and manufacturing a final product differs depending on a variety of factors, such as design complexity, resource allocation, safety requirements, delivery needs, etc. In some cases, once an open-source design is created in-house, or identified elsewhere, the manufacturing process can be relatively quick. “The most important thing is to test the settings, optimize, adapt the design to your local resources, and test with professionals at hospitals. If it works, then you proceed,” said André Rocha, assistant professor at the Escola Superior de Educação de Lisboa, co-coordinator of FabLab Benfica, and an active member of CC Portugal.
“The most important thing is to test the settings, optimize, adapt the design to your local resources, and test with professionals at hospitals.”
For example, a face shield—an important component of personal protection equipment (PPE)—is very “fabricatable,” meaning it’s easy to design and manufacture with a 3D printer, taking around 20 minutes to an hour. Due to the global shortage of face shields, there are many people utilizing open-source designs to manufacture and deliver these to healthcare workers. This includes Darrell Currington, who runs the Rapid Prototyping Centre at OCAD University in Toronto, Canada. “We’re currently working on the production of 3D printed visors which are used to make face shields for hospitals,” he explained over email, “With the university closed down, we weren’t able to run the facility as we normally would. So I decided the best thing we could do was to take what equipment we could, and distribute it among our staff, and faculty that would be most familiar with the technology.”
OCAD University producing 3-D printed protective face shields for hospitals such as @MGHToronto https://t.co/uAysgNQqOx #COVID19 #covidontario pic.twitter.com/wdwAWyzPAb
— OCAD University (@OCAD) April 3, 2020
Although 3D printing is a low-cost and quick way to create PPE components like face shields, there are instances in which it’s better to use other technologies like laser cutting to manufacture more reliable and effective devices—this is especially true for more complex devices like a positive pressure helmet (PPH). A PPH supplies filtered and precise airflow to the wearer. “Imagine an inflatable bubble on your head,” André explained. These have been used in hospitals where COVID-19 cases have overwhelmed the healthcare system, such as Italy. PPHs can relieve the pressure on ventilators and prevent sick people from contaminating the air in crowded hospitals. The process of designing and manufacturing a PPH is more complex than a face shield, requiring more collaboration with industrial companies and medical experts, more materials, and more tests to ensure the hardware is safe and reliable. Therefore, the pace of production and delivery is relatively slow.
André is currently tracking a PPH project launched by the Fab Foundation. The open project’s documentation can be tracked here and the repository is located here.
How are requests received and delivered?
Again, this varies widely depending on the specific context. In some cases, requests are formally channeled through government officials and/or hospital administrators and delivered by established organizations. In other cases, the requests are made informally by healthcare workers and hand-delivered through small volunteer groups or individuals, like Coronavirus Makers in Madrid, Spain. André’s group in Lisbon, Portugal receives PPE supply requests directly from local healthcare workers. “All the help and requests are informal,” he explained, “We [the volunteers] meet remotely almost every day to prepare next day donations to hospitals, police squads, and next developments.”
Aquí una foto que nos hacen llegar unos héroes de un centro de salud de Madrid. Como siempre decimos, ¡¡gracias a vosotros!!#DeEstaSalimosJuntos pic.twitter.com/pukPtWuFdD
— CoronavirusMakers.org (@CoronavirusMak3) April 10, 2020
Unfortunately, volunteer groups and individual efforts suffer from limited capacity and resources—thus, they’re unable to scale their efforts. André and his group are hoping to overcome these challenges by “developing cutting stamps for printing houses that can deliver a few thousand [face shields] in a couple of hours.” However, localized challenges, like a scarcity of the necessary materials to manufacture the supplies, are more difficult to solve. “The effort here is to create versions for different materials, thicknesses, and production processes based on available resources,” he explained.
Are these devices safe?
The landscape of open-source hardware feels a bit like the “wild wild west” due to the urgency and desperation of the current situation. However, ensuring that open-source hardware is safe and reliable is imperative. The devices developed by The Glia Project and their production site, for example, are approved by Health Canada. However, that approval process takes time and resources—neither of which are readily available during a crisis like the COVID-19 pandemic.
In many countries, safety information and regulations around medical devices are publicly available and should be followed.
Therefore, it’s important that manufacturers (even those do-it-yourself hobbyists sewing face masks) do their due diligence in ensuring their products are safe. But how? “I think the most basic level is to test solutions with local health professionals,” emphasized André, “Another is to be extremely careful during fabrication. Everything should be validated by professionals before usage…In projects that represent higher complexity, I believe that [public health] authorities should be involved and contacted.” Darrell’s group, for example, checked with Michael Garron Hospital in Toronto for a tested and approved 3D printed face shield design before starting their efforts. “The hospital had worked with a designer named Shawn Lim, they tested his design, and found they could sanitize the visor and it would be safe for use in their hospital,” Darrell explained, “They then posted the design on their website and asked for anyone with a 3D printer to contribute…As of this evening [April 9] we should have just under 1000 units ready for drop off at the hospital on Tuesday.”
In many countries, safety information and regulations around medical devices are publicly available and should be followed. For example, the United States Federal Drug Administration (FDA) lists regulatory standards for a variety of devices on their website, and in response to COVID-19, they’ve curated specific information on ventilators and PPE.
Where can I find open-source initiatives and designs?
There are hundreds, if not thousands, of different open-source hardware initiatives that you can contribute to and designs that you can utilize. There are a few repositories that you can search through, including Appropedia, Wikifactory, and Public Invention’s “Evaluation of Open Source Ventilators,” as well as loosely organized social media groups to join, including the aforementioned Helpful Engineering Group on Slack and Open Source COVID-19 Medical Supplies (OSCMS) on Facebook. Just One Giant Lab (JOGL) has also launched several projects under their OpenCovid19 Initiative. There are also more country-specific initiatives and designs, such as Breath4Life (Belgium), Un Respiro (Argentina), Fast Jungle Face Shield (Panama), Make4Covid (USA), VentilAid (Poland), Open Source Ventilator (Ireland), OxyGen (Spain), Open Source Against COVID-19 (Belgium).
According to André, it’s important to distinguish ‘pirate’ initiatives that “reverse-engineer medical equipment” from other initiatives developing new designs through more official collaborations and/or partnerships by universities, companies, and research centers. “Information about the latter is unclear because it is hard to distinguish the nature of the initiative,” he emphasized, “We don’t always know if patents will be filed later on or if they are universally available open-source designs.”
 In order to avoid intellectual property (IP) issues, and make it clear the results of these collaborations are open source, Creative Commons is urging individuals, companies, and research institutions to clearly utilize an open-source license or sign the Open COVID Pledge—which grants the public free, temporary access to IP rights in support of solving the COVID-19 crisis, removing obstacles to knowledge and inventions that could save lives and limit suffering.
In order to avoid intellectual property (IP) issues, and make it clear the results of these collaborations are open source, Creative Commons is urging individuals, companies, and research institutions to clearly utilize an open-source license or sign the Open COVID Pledge—which grants the public free, temporary access to IP rights in support of solving the COVID-19 crisis, removing obstacles to knowledge and inventions that could save lives and limit suffering.
P.s. You don’t need to know how to operate a 3D printer, laser cutter, or sewing machine to help out. You can donate materials, money, or your time to each initiative. Just take a look at their websites!
What’s next?
The current situation is not ideal. The explosive growth of open-source hardware over recent weeks is the direct result of devastating medical supply shortages across the world—and unfortunately, current efforts are relatively ad hoc, difficult to scale, and loosely organized. Therefore, it’s impossible to predict what will happen to all of the open-source hardware developed in reaction to COVID-19. Will these designs become legitimate alternatives to those found on the market once the pandemic is over? Will they be used to correct the “mismatch” of medical devices globally? Or will they simply be relegated to the digital archives of history? These are important questions that will need to be examined in the coming months.
For now, let’s get to work. ??
If you have a question regarding CC Licenses and how they apply to hardware designs or the Open COVID Pledge, please feel free to contact us at info@creativecommons.org.
Posted 15 April 2020